Pain in haemophilia
Explore our interactive infographic to understand pain in haemophilia – including types of pain and coping with the impact on daily life.
What is pain?
Pain is the body’s way of saying something isn’t quite right – a warning sign that damage is occurring or about to happen.1,2
Many people with haemophilia have their own personal experience of pain.1 However, it should not be considered the ‘norm’.
Pain can be managed and prevented.1
Types of pain
Pain in haemophilia is often related to bleeding into joints. There are two types – although hard at times, it’s important to tell them apart as they are managed differently.1
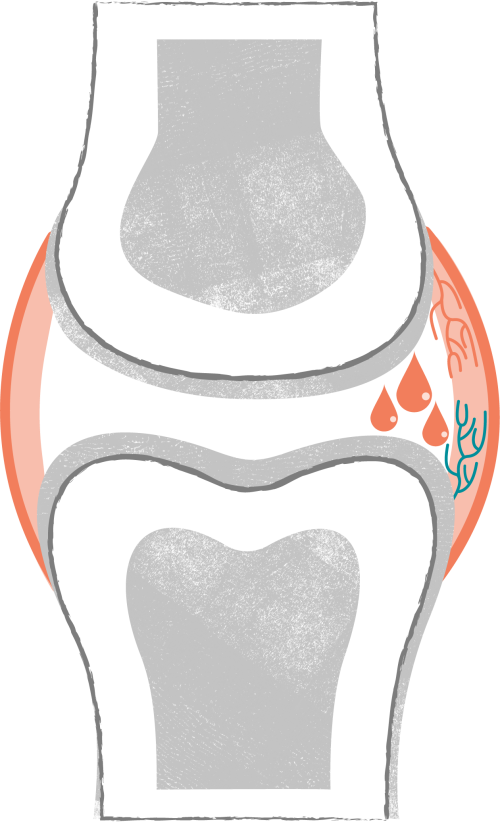
Acute pain1,3–5
- Sudden short-term pain, lasting hours or days
- May feel like throbbing, sharp pain or tenderness
More about acute pain
Acute pain is caused by bleeding into a joint (haemarthrosis) that may happen after an injury.1
During a bleed, the affected joint may swell suddenly, and the area might feel hot, stiff and painful.1,3
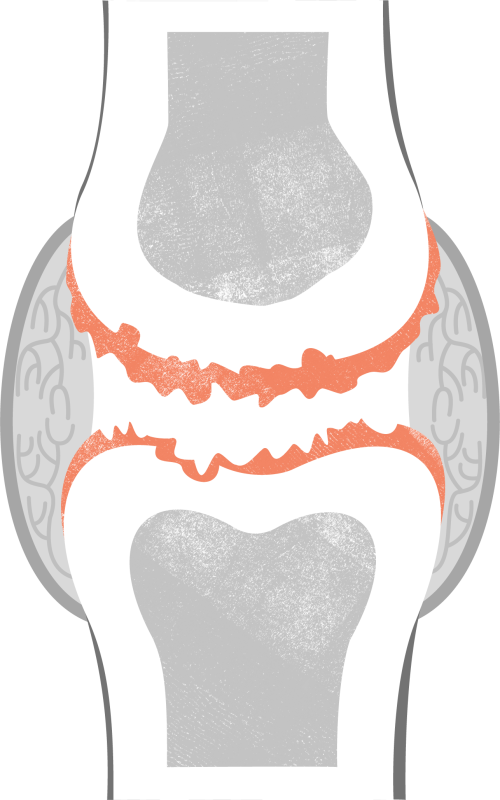
Chronic pain1,3–5
- Persistent longer-term pain, lasting months or longer
- May feel like aching, stiffness or ongoing discomfort
More about chronic pain
Chronic pain is caused by joint damage as a result of repeated bleeds (chronic haemophilic arthropathy).1,4
Joint damage can lead to long-term stiffness, limited movement and chronic pain.1,3,4
Pain sites
Pain can occur where bleeds happen. 1 The most common bleeding sites in haemophilia are the hinge joints (ankles, knees and elbows).6
How can pain be managed?
As they have different causes, acute and chronic pain are managed differently. There are medical and non-medical approaches to help treat both types.1

Acute pain
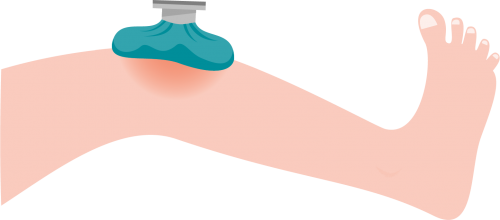
R.I.C.E method (within 24 to 48 hours)4,5,7,8
Protects from further injury and helps reduce bleeding and swelling.
R.I.C.E. can help remind you of the steps to take to help treat an injury:4,5
- Rest the joint and use a splint to limit movement
- Apply ice (in a towel or plastic bag)
- Compress using a bandage or elastic wrap
- Elevate (raise) the affected limb above heart level
Prompt treatment1,8
Acute pain caused by a bleed* typically lessens after treatment with clotting factor therapy.
*Pain can also occur without a bleed.
Following doctor's instructions, treatment should be given as early as possible after a bleed is detected.1,8
Chronic pain

Relaxation techniques4
Help reduce tension and stress.
Hypnosis, meditation and controlled breathing can help cope with pain.4

Surgery1,9,10
To restore or correct the affected joint.
Severe joint damage associated with chronic pain and disability may require orthopaedic surgery.1,9,10
Both pain types

Protection from bleeds1,8
Future bleeds can be prevented with prophylactic therapy.
A review of haemophilia treatment may be helpful if bleeds occur while on prophylactic therapy.

Pain relievers5,8
Over-the-counter or prescription pain relief medicines may be appropriate.
Always seek doctor's advice as certain medicines can interfere with clotting.5,8
Physical therapy4,8,11
Helps manage pain and restore joint function.
Physiotherapists can also teach exercises for recovery at home.11
Coping with pain
Pain is not just a physical discomfort, it’s also an emotional experience1,2 that can have an impact on:

Daily life12
Being less able to carry out everyday tasks.

Connecting with others12,13
Wanting to socialise less with others. Having a low mood (feeling irritable, tense or withdrawn) that impacts relationships.
Enjoying yourself12
Being less involved in usual leisure activities.

Personal growth12,13
Feeling less productive and needing to take time off work or study.
Staying on top of mental health
Everyone experiences and copes with pain differently.1 Pain can lead to negative emotions,5,13 which in turn can cause pain to feel worse.1,14 Below are some tips that could help you keep on top of things.
Self-help & ways to take charge
Engage in low-intensity exercise4,11,14
Easing into a routine that suits you can help improve mood, mobility and pain.
Sleep well14,15
A good night’s sleep boosts mood. If you struggle to sleep because of pain, ask your healthcare team for support.

Find a way to relax and reduce tension4,14
Meditating or breathing exercises won’t necessarily make the pain go away but may help you cope.

Stay in control1,13
Unhealthy behaviours to help cope with pain (for example, becoming dependent on substances) can lead to other health issues. If you relate to this, speak with your doctor as soon as possible.
Get your team involved
You should not feel like you have to ‘put up’ with pain or face it alone. Try to open up with your haemophilia care team about how you are feeling. They can help provide psychological support and may prescribe medicine to help.8,13,16
If you would like to learn more about how to live well with haemophilia, you can explore information, advice and stories at LiberateLife.eu
Any medical information is for informational purposes only and is not a replacement for advice given by a physician or other medical professionals.
- Auerswald G, et al. Pain and pain management in haemophilia. Blood Coagul Fibrinolysis 2016;7(8):845–854. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5087566/ (accessed June 2021).
- Yam MF, et al. General pathways of pain sensation and the major neurotransmitters involved in pain regulation. Int J Mol Sci 2018;19(8):2164. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6121522/ (accessed June 2021).
- Rambod M, et al. Pain: the voiceless scream in every haemophilia patient’s life. J Haem Pract 2016;3(1). Available at https://www.researchgate.net/publication/292178219_Pain_the_voiceless_
scream_in_every_hemophilia_patient's_life (accessed June 2021). - Riley RR, et al. Assessment and management of pain in haemophilia patients. Haemophilia 2011;17(6):839–845. Available at https://pubmed.ncbi.nlm.nih.gov/21645179/ (accessed June 2021).
- Steps for living (Hemophilia). Pain management. Available at: www.stepsforliving.hemophilia.org/step-out/non-factor-treatment/pain-management (accessed June 2021).
- National Hemophilia Foundation. Nursing Working Group – nurses’ guide to bleeding disorders. Common bleeding episodes. Available at: https://www.hemophilia.org/sites/default/files/document/files/nurses-guide-chapter-4-common-bleeding-episodes.pdf (accessed June 2021).
- National Hemophilia Foundation. Physical therapy practice guidelines for persons with bleeding disorders: Joint bleeds. Available at: https://www.hemophilia.org/sites/default/files/document/files/238ptguidelines.pdf (accessed June 2021).
- World Federation of Hemophilia. Guidelines for the management of hemophilia – 3rd edition. Available at: https://www1.wfh.org/publications/files/pdf-1863.pdf (accessed June 2021).
- Rizzo AR, et al. Orthopaedic procedures in haemophilia. Clin Cases Miner Bone Metab 2017;14(2):197–199. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5726209/ (accessed June 2021).
- Carlos Rodriguez-Merchan, E. What’s new in orthopedic surgery for people with hemophilia. Arch Bone Jt Surg 2018;6(3):157-160. Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5990719/ (accessed June 2021).
- World Federation of Hemophilia. Exercises for people with hemophilia. Available at: www1.wfh.org/publications/files/pdf-1302.pdf (accessed June 2021).
- Dueñas M. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res 2016;9:457–467. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4935027/ (accessed June 2021).
- World Federation of Hemophilia. Psychosocial care for people with haemophilia. Available at: www1.wfh.org/publications/files/pdf-1198.pdf (accessed June 2021).
- NHS Scotland. Chronic pain: a self help guide. Available at: www.nhsinform.scot/illnesses-and-conditions/mental-health/mental-health-self-help-guides/chronic-pain-self-help-guide (accessed June 2021).
- NHS. Live well: Sleep and tiredness. Available at: www.nhs.uk/live-well/sleep-and-tiredness/why-lack-of-sleep-is-bad-for-your-health/ (accessed June 2021).
- Haemophilia Wales. What is a psychologist doing in the haemophilia centre? Available at: www.haemophiliawales.org/psychology-haemophilia (accessed June 2021).